Jeffrey Karp, PhD
Bioengineer, Brigham and Women’s Hospital
Professor of Medicine, Harvard Medical School
Medical Executive Board, Stepping Strong Center
Nitin Joshi, PhD
Associate Bioengineer, Brigham and Women’s Hospital
Instructor of Medicine, Harvard Medical School
Bruce David Levy, MD
Chief, Division of Pulmonary and Critical Care Medicine, Brigham and Women’s Hospital
Parker B. Francis Professor, Harvard Medical School
Yohannes Tesfaigzi, PhD
Researcher, Division of Pulmonary and Critical Care Medicine, Brigham and Women’s Hospital
Member of the Faculty of Medicine, Harvard Medical School
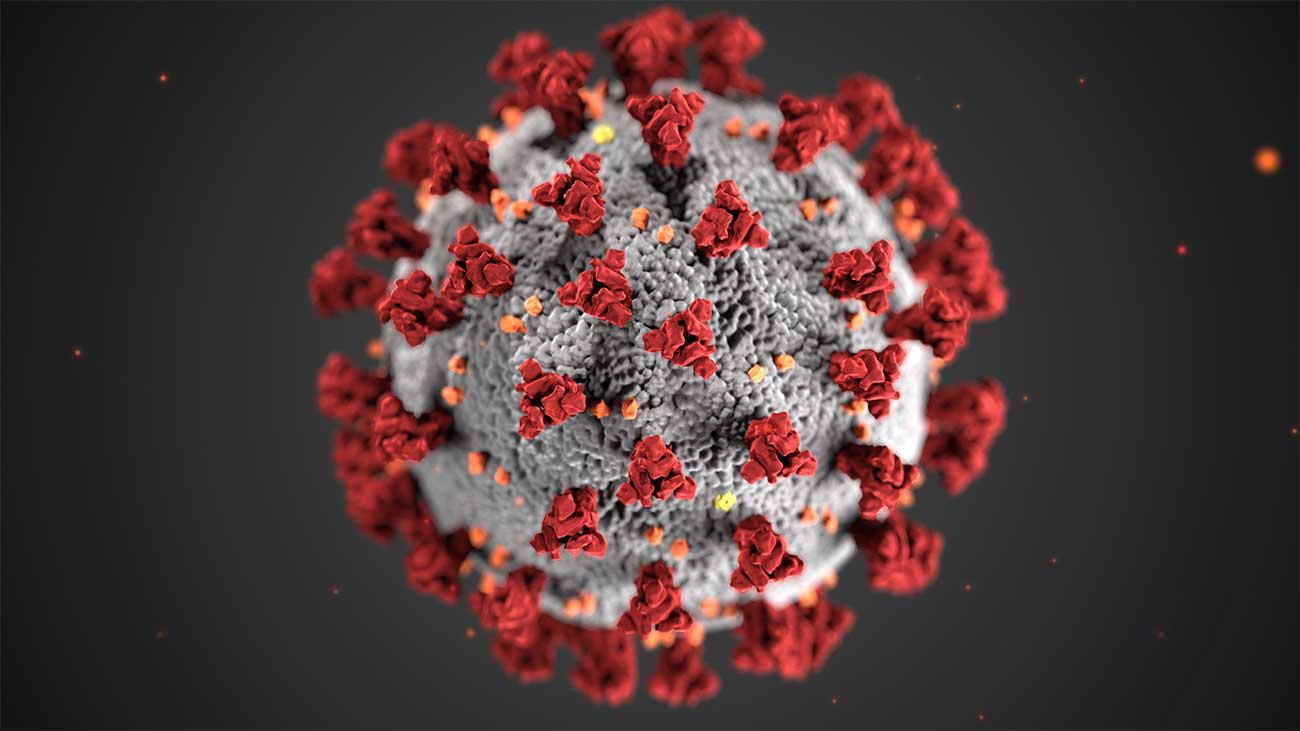
The overall goal of this project is to develop a nasal spray formulation to capture and deactivate the respiratory pathogens in the nasal cavity, thereby preventing transmission of SARS-CoV-2.
During the course of the team’s investigation over the last six months, they finetuned the unique combination of materials needed for the nasal spray – which were already recognized as safe by the FDA — and identified ideal concentration ranges via multiple screening experiments that aimed to maximize sprayability, mucoadhesiveness, and anti-viral properties while capturing respiratory droplets. The optimized formulation demonstrated >99% killing of Influenza A and SARS-CoV-2 viruses within minutes of contact time, as suggested by in vitro antiviral assays. The team also demonstrated that the formula can kill >99% of E. coli bacteria within minutes.
Recognizing that maximizing the capture of respiratory droplets is critical to ensuring the efficacy of the nasal spray, investigators used a 3D printed model of a human nasal cavity for a series of experiments. Findings revealed that the formulation doubles the capture of large respiratory droplets when sprayed into the nose. A single dose of the formulation administered into the nasal cavity in mice results in more than eight hours of exposure, which is much higher than previously developed nasal formulations. Spray characteristics of the team’s nasal formulation are within the ideal ranges, as defined previously for nasal sprays.
The team is currently validating the efficacy of the formulation in mice and expects to translate this into an over-the-counter product within the next six months.
Prevention of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) transmission is one of the critical aspects of clinical management of COVID-19. The predominant mode of transmission of this virus is through inhalation of contaminated aerosols. The inhaled virus attaches to the nasal lining, where it multiplies and gets into airways through specific cell types, including goblet cells in the nasal mucosa. Given that the nasal mucosa is a major entry point for SARS-CoV-2, we propose to develop an easy-to-use nasal spray that can: (1) form a hydrogel barrier on nasal mucosa, thereby capturing the inhaled viruses; and (2) release virucidal agents that can also deactivate the virus immediately.
The team envisions that this approach can provide an additional layer of personal protection over conventionally used protective equipment including surgical masks or N95 respirators, while integrating seamlessly into our daily lives. The hydrogel can also hydrate nasal lining, which can promote nose breathing—a factor that previously has been shown to assist in the deactivation of inhaled pathogens.
The team was working on nasal spray formulations in a different context. But recently, with the COVID-19 pandemic, they realized that this technology can be tuned to potentially prevent transmission of SARS-CoV-2 infection.
 Jeff Karp, PhD, is a bioengineer at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School. He is also a principal faculty member at the Harvard Stem Cell Institute and serves as affiliate faculty member at the Broad Institute and the Harvard-MIT Division of Health Sciences and Technology. Karp works in the fields of drug delivery, medical devices, stem cell therapeutics, and tissue adhesives. He has published over 125 peer-reviewed papers, with more than 20,500 citations, and has given over 300 invited lectures. He has more than 100 issued or pending national and international patents. Several technologies developed in his lab have led to multiple products currently in development or on the market and for the launch of seven companies that have raised over $300 million in funding. Technologies include high tech skincare, tissue adhesives and 3D printed biomedical devices, immunomodulation with biologically responsive materials, small molecule regenerative therapeutics with an initial target of hearing loss, cannabinoid therapeutics, biomedical devices to improve child safety, needles that automatically stop when they reach their target, and a bioengineered luminal coating for controlled GI targeting.
Jeff Karp, PhD, is a bioengineer at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School. He is also a principal faculty member at the Harvard Stem Cell Institute and serves as affiliate faculty member at the Broad Institute and the Harvard-MIT Division of Health Sciences and Technology. Karp works in the fields of drug delivery, medical devices, stem cell therapeutics, and tissue adhesives. He has published over 125 peer-reviewed papers, with more than 20,500 citations, and has given over 300 invited lectures. He has more than 100 issued or pending national and international patents. Several technologies developed in his lab have led to multiple products currently in development or on the market and for the launch of seven companies that have raised over $300 million in funding. Technologies include high tech skincare, tissue adhesives and 3D printed biomedical devices, immunomodulation with biologically responsive materials, small molecule regenerative therapeutics with an initial target of hearing loss, cannabinoid therapeutics, biomedical devices to improve child safety, needles that automatically stop when they reach their target, and a bioengineered luminal coating for controlled GI targeting.
 Nitin Joshi, PhD, is an associate bioengineer at Brigham and Women’s Hospital and an instructor of medicine at Harvard Medical School. Dr. Joshi’s prime research focus is drug delivery and biomaterials. Technologies developed by Dr. Joshi have been published, patented and licensed and are currently in clinical trials. He was recognized by MIT’s Technology Review Magazine (TR35) as being one of the top innovators in India and was also awarded the prestigious Lockheed Martin Innovation award for his work. Dr. Joshi’s work has been highlighted in multiple media outlets and scientific journals around the world including Science Daily, Journal of American Medical Association (JAMA), Fierce Biotech, Medical Xpress and Nature Reviews Rheumatology.
Nitin Joshi, PhD, is an associate bioengineer at Brigham and Women’s Hospital and an instructor of medicine at Harvard Medical School. Dr. Joshi’s prime research focus is drug delivery and biomaterials. Technologies developed by Dr. Joshi have been published, patented and licensed and are currently in clinical trials. He was recognized by MIT’s Technology Review Magazine (TR35) as being one of the top innovators in India and was also awarded the prestigious Lockheed Martin Innovation award for his work. Dr. Joshi’s work has been highlighted in multiple media outlets and scientific journals around the world including Science Daily, Journal of American Medical Association (JAMA), Fierce Biotech, Medical Xpress and Nature Reviews Rheumatology.
