Our goal with the Stepping Strong Injury Prevention program is to enhance collaborations across existing injury prevention programs at the Brigham and beyond, and to prevent injuries through outreach, research, training and education, and advocacy.
This web page highlights program partners, descriptions, and contact information for our diverse injury prevention initiatives. For more information, contact Cheryl Lang.
 Maria Tumang, the Injury Prevention Coordinator in the Division of Trauma, Burn, and Surgical Critical Care, is bringing a fun and affordable way to improve health and quality of life for those most at risk of falls through a program called Bingocize®. This socially engaging group-based program combines exercise, health education, and the widely popular game of bingo. In addition to Bingocize®, Maria also leads Tai Chi for Falls Prevention, another evidence-based fall prevention program focusing on building strength, flexibility, and balance.
Maria Tumang, the Injury Prevention Coordinator in the Division of Trauma, Burn, and Surgical Critical Care, is bringing a fun and affordable way to improve health and quality of life for those most at risk of falls through a program called Bingocize®. This socially engaging group-based program combines exercise, health education, and the widely popular game of bingo. In addition to Bingocize®, Maria also leads Tai Chi for Falls Prevention, another evidence-based fall prevention program focusing on building strength, flexibility, and balance.
Learn more about the Bingocize program
Contact Maria Tumang to learn more about fall prevention and outreach.
 Innovator Award recipient Cornelia Griggs, MD, is a pediatric surgeon at Massachusetts General Hospital, the director of education at the MGH Center for Gun Violence Prevention, and a passionate advocate for preventing gun violence. We caught up with Dr. Griggs to discuss her Stepping Strong-funded project—Developing and evaluating an avatar/virtual reality-based gun violence prevention training program for clinicians—and the importance of using a public health approach to unravel the challenge of gun violence in the U.S.
Innovator Award recipient Cornelia Griggs, MD, is a pediatric surgeon at Massachusetts General Hospital, the director of education at the MGH Center for Gun Violence Prevention, and a passionate advocate for preventing gun violence. We caught up with Dr. Griggs to discuss her Stepping Strong-funded project—Developing and evaluating an avatar/virtual reality-based gun violence prevention training program for clinicians—and the importance of using a public health approach to unravel the challenge of gun violence in the U.S.
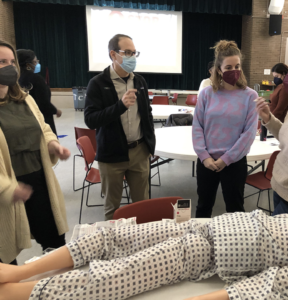 An estimated 100,306 drug overdose deaths occurred in the U.S. in 2021. In Massachusetts alone, 2,000 citizens die each year due to opioid use disorder. In this interview, Scott Weiner, MD, MPH—emergency physician and medical director of the Brigham Comprehensive Opioid Response and Education and Quality and Safety programs—talks about a new Stepping Strong-funded program that trains lay people to reverse opioid deaths.
An estimated 100,306 drug overdose deaths occurred in the U.S. in 2021. In Massachusetts alone, 2,000 citizens die each year due to opioid use disorder. In this interview, Scott Weiner, MD, MPH—emergency physician and medical director of the Brigham Comprehensive Opioid Response and Education and Quality and Safety programs—talks about a new Stepping Strong-funded program that trains lay people to reverse opioid deaths.
 Congratulations to the Brigham and Women’s Hospital Burn Center team for recently receiving reverification as an adult burn center by the American Burn Association and the American College of Surgeons Committee on Trauma. Under the direction of Anupama Mehta, MD, the burn care team has extensive experience managing severe burns and smoke inhalation. providing critical treatment such as resuscitation and wound care, conducting community outreach on burn prevention, and pursuing cutting-edge research to improve the treatment of burn injuries. Notably, the Burn Center won the Brigham and Women’s Hospital 2021 McGraw Opioid Innovator Award for their project entitled, “Can Olfactory Virtual Reality Reduce Opioid Consumption and Improve Tolerance in Burn Patients Undergoing Dressing Changes?”
Congratulations to the Brigham and Women’s Hospital Burn Center team for recently receiving reverification as an adult burn center by the American Burn Association and the American College of Surgeons Committee on Trauma. Under the direction of Anupama Mehta, MD, the burn care team has extensive experience managing severe burns and smoke inhalation. providing critical treatment such as resuscitation and wound care, conducting community outreach on burn prevention, and pursuing cutting-edge research to improve the treatment of burn injuries. Notably, the Burn Center won the Brigham and Women’s Hospital 2021 McGraw Opioid Innovator Award for their project entitled, “Can Olfactory Virtual Reality Reduce Opioid Consumption and Improve Tolerance in Burn Patients Undergoing Dressing Changes?”
To learn more about the Burn Center and related resources:
 As a freshman in college, Ali Salim, MD (second from left), had to walk through Duke University Hospital to get to the main campus for classes. He had never been exposed to medicine before, but because of this daily exposure, he decided to volunteer in the emergency room. Once there, he watched and learned—an experience that ultimately led to his focus on improving outcomes for trauma patients. In this interview, Dr. Salim shares his passion for decreasing preventable traumatic injuries and talks about his long-term vision for the Stepping Strong Injury Prevention Program.
As a freshman in college, Ali Salim, MD (second from left), had to walk through Duke University Hospital to get to the main campus for classes. He had never been exposed to medicine before, but because of this daily exposure, he decided to volunteer in the emergency room. Once there, he watched and learned—an experience that ultimately led to his focus on improving outcomes for trauma patients. In this interview, Dr. Salim shares his passion for decreasing preventable traumatic injuries and talks about his long-term vision for the Stepping Strong Injury Prevention Program.
 In addition to directing the Stepping Strong Injury Prevention program, Molly Jarman, PhD, MPH, is a lead investigator at the Center for Surgery and Public Health and an assistant professor at Harvard Medical School. Her research addresses trauma surgery and emergency medical services, with primary interest in trauma system organization and access to care for underserved populations. In this interview Jarman speaks about her focus on multifaceted, multidisciplinary approaches to preventing injuries. .
In addition to directing the Stepping Strong Injury Prevention program, Molly Jarman, PhD, MPH, is a lead investigator at the Center for Surgery and Public Health and an assistant professor at Harvard Medical School. Her research addresses trauma surgery and emergency medical services, with primary interest in trauma system organization and access to care for underserved populations. In this interview Jarman speaks about her focus on multifaceted, multidisciplinary approaches to preventing injuries. .
 The Brigham Health Bridge Clinic opened its doors in April 2018 to provide rapid (often same day) low-barrier access to patients with all types of substance use disorders (SUDs). Under the direction of Samata Sharma, MD, the clinic provides comprehensive addiction care for patients referred through inpatient services, the Emergency Department, and primary/specialty care practices. Multidisciplinary physicians from departments including addiction psychiatry, addiction medicine, infectious disease, and women’s health treat the underlying SUD with medications while social worker connects patients with services such as housing, food benefits, transportation, and recovery coaches who provide peer support as patients engage in treatment. After receiving this initial care—typically from three to six months—many patients reach a more stable stage of their recovery and are then “bridged,” or connected, to a practice or program that best meets their needs to maintain long-term recovery.
The Brigham Health Bridge Clinic opened its doors in April 2018 to provide rapid (often same day) low-barrier access to patients with all types of substance use disorders (SUDs). Under the direction of Samata Sharma, MD, the clinic provides comprehensive addiction care for patients referred through inpatient services, the Emergency Department, and primary/specialty care practices. Multidisciplinary physicians from departments including addiction psychiatry, addiction medicine, infectious disease, and women’s health treat the underlying SUD with medications while social worker connects patients with services such as housing, food benefits, transportation, and recovery coaches who provide peer support as patients engage in treatment. After receiving this initial care—typically from three to six months—many patients reach a more stable stage of their recovery and are then “bridged,” or connected, to a practice or program that best meets their needs to maintain long-term recovery.
 The Brigham’s Falls Prevention Outreach program is led by the injury prevention coordinator in the Division of Trauma, Burn, and Surgical Critical Care. The Injury Prevention coordinator hosts a series of workshops including two evidence-based falls prevention programs:
The Brigham’s Falls Prevention Outreach program is led by the injury prevention coordinator in the Division of Trauma, Burn, and Surgical Critical Care. The Injury Prevention coordinator hosts a series of workshops including two evidence-based falls prevention programs:
- Tai Chi for Arthritis
- A Matter Balance
Through these programs, the coordinator works with older adults in the Boston area to reduce their risk of injury from falling and with a goal of improving their strength, flexibility, and balance. Our Falls Prevention Outreach efforts help participants maintain their health and independence by preventing falls and resulting injuries.
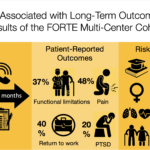 The Functional Outcomes and Recovery After Trauma Emergencies (FORTE) project, led by Ali Salim, MD, and Juan Herrera-Escobar, MD, evaluates outcomes of patients recovering from traumatic injuries at three Level One trauma centers in Boston: Brigham and Women’s Hospital, Massachusetts General Hospital, and Boston Medical Center. The FORTE study is taking a new approach to evaluating trauma-related outcomes. Rather than simply looking at mortality and morbidity at 30 days, which is the current practice, FORTE seeks to expand our knowledge of trauma outcomes by checking in with patients at six months to a year post-injury. In doing so, the FORTE team is continuously improving a database of long-term patient-reported outcomes to measure factors including functional status, quality of life, symptoms, and treatment adherence.
The Functional Outcomes and Recovery After Trauma Emergencies (FORTE) project, led by Ali Salim, MD, and Juan Herrera-Escobar, MD, evaluates outcomes of patients recovering from traumatic injuries at three Level One trauma centers in Boston: Brigham and Women’s Hospital, Massachusetts General Hospital, and Boston Medical Center. The FORTE study is taking a new approach to evaluating trauma-related outcomes. Rather than simply looking at mortality and morbidity at 30 days, which is the current practice, FORTE seeks to expand our knowledge of trauma outcomes by checking in with patients at six months to a year post-injury. In doing so, the FORTE team is continuously improving a database of long-term patient-reported outcomes to measure factors including functional status, quality of life, symptoms, and treatment adherence.
To date, the FORTE team has completed 3,536 follow-up interviews with 2,836 trauma survivors. It has also published 13 manuscripts in peer-reviewed surgical journals spanning multiple areas, including mental, physical, and social health outcomes research. FORTE is also applying for R-01 funding and planning to expand to other trauma centers across the country. By interviewing patients during their first year following their injury, we are learning more about the long-term challenges people face as they recover from traumatic injury. The FORTE project can ultimately help patients and providers to predict long-term outcomes about a specific injury and inform decisions of healthcare. For more information, contact Juan Herrera-Escobar, MD or visit the FORTE website.
 The Stepping Strong Screening, Brief Intervention, and Referral to Treatment Program (SBIRT)
The Stepping Strong Screening, Brief Intervention, and Referral to Treatment Program (SBIRT)
Harmful alcohol use affects millions of adults across the United States each year. Fortunately, however, data from the United States Preventive Services Task Force (USPSTF) reveals that early detection of alcohol use through screening tools, followed by counseling intervention, may prevent harmful alcohol use.
Recently, the Brigham mandated that all trauma patients be screened with the Alcohol Use Disorders Identification Test, or Audit C—an alcohol screening protocol identified by the USPSTF as one of the most accurate screening tools available. All Brigham patients who screen positive, therefore, must receive a brief intervention and referral to services. Brigham’s Trauma Division has a mandatory goal of screening 80 percent of patients upon admission and providing substance use intervention to 100 percent of those patients who screened positive.
 Superior Surgical and Trauma Care for Seniors Pathway (SSTEP)
Superior Surgical and Trauma Care for Seniors Pathway (SSTEP)
Older patients face a unique set of health challenges—including chronic fatigue, low muscle mass, cognitive impairment, bone fractures, and reduced mobility—that can raise their risk of illness or injury during hospitalization.
According to Zara Cooper, MD, MSc, a member of the Stepping Strong medical executive committee and director of the Brigham’s Center for Surgery and Public Health, “Frailty and cognitive impairment are often key contributing factors in falls and accidents that lead to fractures and other injuries among older patients. We believe that focusing on these underlying conditions is essential to optimizing care and outcomes.”
Launched in 2016, the Brigham’s SSTEP Pathway (formally called the BWH Frailty Identification and Care Pathway) is a multidisciplinary program that addresses challenges for elderly patients by providing clinicians with standardized guidelines for identifying and accommodating frailty—a complex, often age-related syndrome characterized by physical decline and increased vulnerability to stressors.
The SSTEP Pathway screens patients aged 65 years or older for frailty to determine whether they are frail or at risk of becoming frail. If screened positive for frailty, patients receive geriatric-centered orders aimed at preventing delirium and improving function. Additionally, SSTEP patients are seen by experts in gerontology, nutrition, and physical therapy.
Read an article about how the pathway has lowered readmission rates in older adult trauma patients.
Contact Lynne O’Mara to learn more about SSTEP program.
 The Center for Community Health and Health Equity Violence Intervention Programs
The Center for Community Health and Health Equity Violence Intervention Programs
The Brigham’s Center for Community Health and Health Equity (CCHHE) was established in 1991 to develop, implement, manage, and evaluate initiatives that minimize health inequities and improve the well-being of those living in its priority neighborhoods of Dorchester, Jamaica Plain, Mattapan, Mission Hill, and Roxbury. CCHHE focus areas include eliminating inequities in infant mortality and cancer care; supporting young parents; promoting youth development and employment through education and career opportunities; and curbing and responding to community, domestic, and interpersonal violence. Three CCHHE programs are highlighted below.
- Violence Recovery Program. According to Program Director Mardi Chadwick Balcom, “Our goal with the Violence Intervention and Prevention program is to reduce the burden of violence in Boston by providing comprehensive services to patients and families admitted to the Brigham after sustaining any violent intentional injury.” A collaboration between CCHHE and the Division of Trauma, Burn and Surgical Critical Care, the program includes a multidisciplinary team of violence recovery advocates and a mental health clinician who support patients and families both during hospitalization and after discharge. To reach an advocate page #32063 or email violenceintervention@partners.org for non-emergency referrals.
- Passageway Program. The Passageway Program is a domestic violence advocacy program that provides support to people experiencing abuse from an intimate partner. Advocates are available to respond in real time to ambulatory patients, in-patients, and providers on the Brigham main campus, at Brigham and Women’s Faulkner Hospital, and at Southern Jamaica Plain and Brookside Community health centers. Passageway advocates work with patients, employees, and community members to develop and support safe, collaborative interventions to domestic violence. Services include safety planning, individual counseling, crisis intervention, referrals to community resources, and medical, legal, and courts advocacy, and referrals to community resources. Advocates are committed to connecting with patients where they are, and all services are free, voluntary, and confidential. To speak with an advocate, call 617-732-8753, page #31808, or email passageway@partners.org for non-emergencies.
- Jamaica Plain Neighborhood Trauma Team (JPNTT). The JPNTT provides response and recovery services to individuals and communities experiencing trauma due to community violence in the neighborhood of Jamaica Plain. Services include individual and family support, short-term case management, coping/healing groups, community engagement, support, and informational sessions. A collaborative partnership, JPNTT is one of five Neighborhood Trauma Teams that participate in a city-wide network of hospitals, police departments, and youth and family servicing organizations committed to addressing the burden of community. To reach JPNTT, please call or text Sade Smith at 617-835-9222 or email sjonessmith@bwh.harvard.edu. To reach the Neighborhood Trauma Team 24/7 hotline, call 617-431-0125.

