MIT Innovator Award Recipient Creates Scalable Color-Changing Compression Bandages
Painful leg ulcers, hematoma, and burn-related scars are among the many challenges faced by patients who sustain traumatic injuries. In this interview, MIT Professor Mathias Kolle and Ben Miller, a doctoral student in MIT’s Department of Mechanical Engineering, explain how an exciting new technology that uses bio-inspired color-changing fibers can help healthcare professionals precisely assess bandage pressure, potentially shortening treatment duration, increasing therapy success rate, and decreasing soaring medical costs.
DW: Mathias and Ben, thanks for talking with me this afternoon. Mathias, back in 2018, you received an Innovator Award for a project called, “Revealing optimal pressure in compression therapy using color-changing fibers.” Can you talk about the origins of this research and what you were trying to accomplish?
MK: Sure. When I started MIT, I was playing with color dynamic materials with the idea of connecting mechanics and optics. I wondered at the time if this technology could be useful in a healthcare setting. So, I contacted [Stepping Strong Director of Innovation and Strategy] Matt Carty and the idea to use color-changing fibers as pressure indicators in bandages came up in a brainstorming session. Matt shared that medical professionals struggle to correctly assess bandage pressure, an issue that can lead to prolonged treatments for those who are healing from traumatic injuries.
DW: Can you give us some examples of how color-changing bandages might work in practice?
MK: There are many conditions where pressure is a variable for treating trauma patients. One example is exerting the right amount of pressure to prevent scarring following reconstructive surgery. Or say a patient suffers from venous ulcers or venous insufficiencies. In that case, the fluid transport up the veins is not proceeding as it should be. The danger is there’s a potential for fluid accumulating in the lower limbs, creating really mean ulcers. Lymphatic disorders that lead to lymphedema can also lead to fluids accumulating in the wrong places. The right amount of pressure can help push the fluids back out of tissue regions where they don’t belong.
“There are many conditions where pressure is a variable for treating trauma patients… When fluids accumulate in the wrong places, the right amount of pressure can help push the fluids out of tissue regions where they don’t belong.”
DW: How did those brainstorming sessions with Matt Carty inform your research?
MK: Those early conversations with Matt got me into this mindset of thinking, okay, what can we do on the mechanical engineering side for things to improve outcomes for trauma patients?
And at some point, Matt encouraged me to apply for the Stepping Strong Innovator Award. Thankfully, I won the award in 2018 and had the opportunity to present my ideas to the Stepping Strong Advisory Board. There were so many bright people in the room! One of the things we discussed was how I intended to scale the technology for this material. Now, because of Ben’s amazing achievements, I think we finally have a solution that can have a real impact.
DW: Ben, can you go into more detail about the scaling problem and how you solved it?
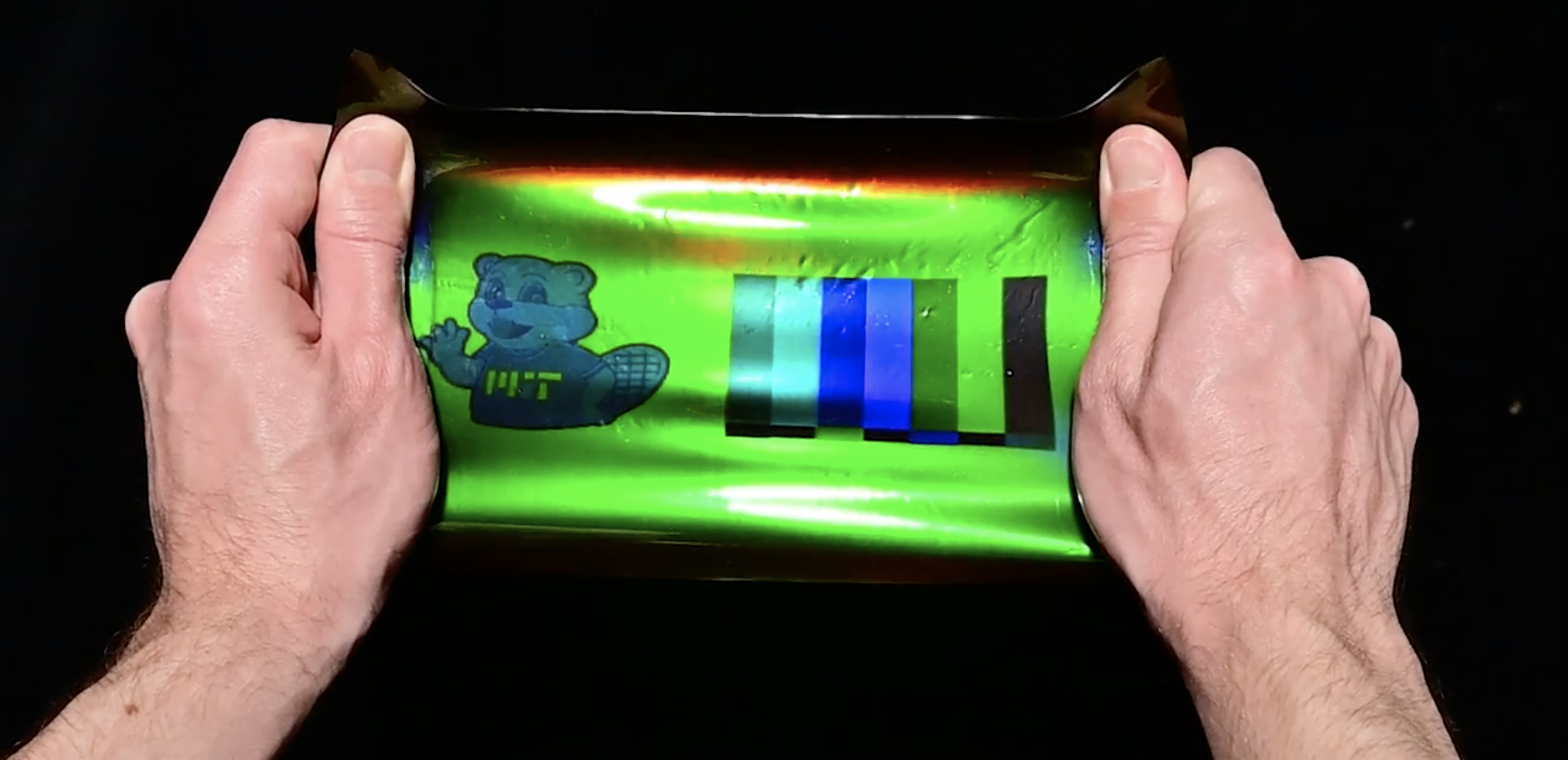
BM: As Mathias mentioned, our team knew from the start that scaling would be an issue with the initial photonic fiber approach. The question we faced was, how can you make a lot of this material cheaply and quickly? Previously, although we were able to test the bandages and make samples in the lab, making 100 bandages was out of the question.
When I first started working for Mathias, I was working on a different project with a similar concept, but a very different application. And then, almost accidentally, I developed a technique that could make a material just like the one Mathias and his previous students envisioned, but lots of it, and very quickly.
DW: What was the accidental discovery, and how did it propel the project forward?
BM: I happened to speak to someone from the MIT Museum about holography, a technique that produces three-dimensional images by superimposing two light beams onto a physical material. I realized what they do in holography is kind of the same thing that nature does with structural color.
That led me to learn more about holography and its history, which in turn led me back to the late 1800s, and an early color photography technique invented by a physicist named Gabriel Lippmann, who later won the Nobel Prize in Physics for the technique.
We realized that combining Lippmann’s original work with modern materials provided a route to a scalable manufacturing process, which also had the benefit of being highly tunable for different applications.
DW: Very cool. Now that you’ve sorted out how to scale the smart material technology, what are the next steps?
MK: We are currently part of a program at the MIT Deshpande Center for Technological Innovation, which has helped to drive our vision of creating a start-up that will bring our pressure indicators to market. Right now, we are refining our business case, running customer interviews, and building our pitch to convince investors that our technology would be useful and commercially viable. Hopefully, we will have more exciting news to share with you soon.
DW: Ben, what other applications are possible with this innovative technology?
BM: I am really excited about the compression therapy application because it is such a clear problem with a clear need. But as you implied, the bandages are only one application. Now that we’ve cleared this scaling hurdle, there are several things that I’ve been focusing on: One is designing clothing that responds to the wearer, to their movements. Another is developing athletic gear that gives you visual feedback regarding your performance or posture. Then there’s robotics. I can imagine using this material to make robotic skin with a human-like sense of touch and creating touch-sensing devices for things like virtual and augmented reality or medical training. It’s a big space we’re looking at now.
“I can imagine using this material to make robotic skin with a human-like sense of touch and creating touch-sensing devices for things like virtual augmented reality or medical training. It’s a big space we’re looking at now.”
DW: This is such a fascinating project. Thank you both for taking the time to speak to me. Any last thoughts?
MK: Being honored with the Stepping Strong Innovator Award back in 2018 has been game-changing, and I am very grateful to be in the Stepping Strong family. Not only have we been able to prove that bandage pressure indication can be useful in a healthcare setting; it has led to our publication in Nature Materials; it has provided us with the means to push this technology further in terms of scaling and application context; and it has brought us to a point where there is potential for real impact.