Empowering Community Partners to Administer Narcan: An Interview with Emergency Physician Scott Weiner
An estimated 100,306 drug overdose deaths occurred in the U.S. in 2021. In Massachusetts alone, 2,000 citizens die each year due to opioid use disorder. In this interview, Donna Woonteiler speaks to Scott Weiner, MD, MPH–emergency physician and medical director of the Brigham Comprehensive Opioid Response and Education and Quality and Safety programs at Brigham and Women’s Hospital–about a new Stepping Strong-funded program that empowers lay people to reverse opioid deaths.
DW: Welcome Dr. Weiner. Let’s start by setting some context for our readers. What problems are you trying to solve with the Stepping Strong Lay Empowerment program?
SC: Broadly speaking, we want to provide our community partners—a lay population with limited medical training–access to and training in lifesaving skills and techniques. I’m specifically focused on teaching laypeople how to use Narcan (also known as naloxone) to reverse overdoses.
DW: I read that once a person becomes addicted to opioids, options for treatment are limited by a hard-to-navigate system.
SC: That’s correct. The U.S. is in the midst of an opioid epidemic, and Massachusetts has suffered disproportionately. This crisis affects everyone–young and old, rich and poor, and all races.
“Over a decade, the military trained and empowered soldiers, sailors, airmen, and Marines to recognize life-threatening bleeding, apply pressure, pack a wound, or apply a tourniquet. Pre-hospital hemorrhage control, intervention, blood transfusions, and rapid prehospital transport reduced deaths by 44% on the battlefield, which equated to thousands of lives saved.”
We know that prescribers are partially responsible for the crisis. We also know that patients have a poor understanding of the safety of opioids. Lastly, as you said, we have a fragmented system that makes it challenging for someone to get help in their time of need.
DW: What services at the Brigham are available to address the crisis?
SC: I was fortunate to start a program called B-CORE–the Brigham Comprehensive Opioid Response and Education Program–which aims to address all aspects of opioids as they relate to patients and our Brigham community. The project is designed to improve access to treatment for patients with opioid use disorder, educate the community on the safe use of opioids, improve access to Narcan, and offer guidelines to prescribers.
So it seemed like a natural fit to reach out directly to Stepping Strong’s community partners and offer training in administering Narcan.
DW: Who are our community partners, and why do they need this program?
SC: To start with, we believe that everyone can benefit from knowing how to reverse overdose through administering Narcan. However, the training is particularly beneficial to those who live in communities with greater exposure to violence and substance use.
That said, our partners are community-based organizations who serve individuals who are affected by systemic generational urban poverty, violence, and substance use. Thus far we have completed one training with YouthConnect and will be training Boston Uncornered in April.
DW: Got it. Can you go into a little more detail about what you teach?
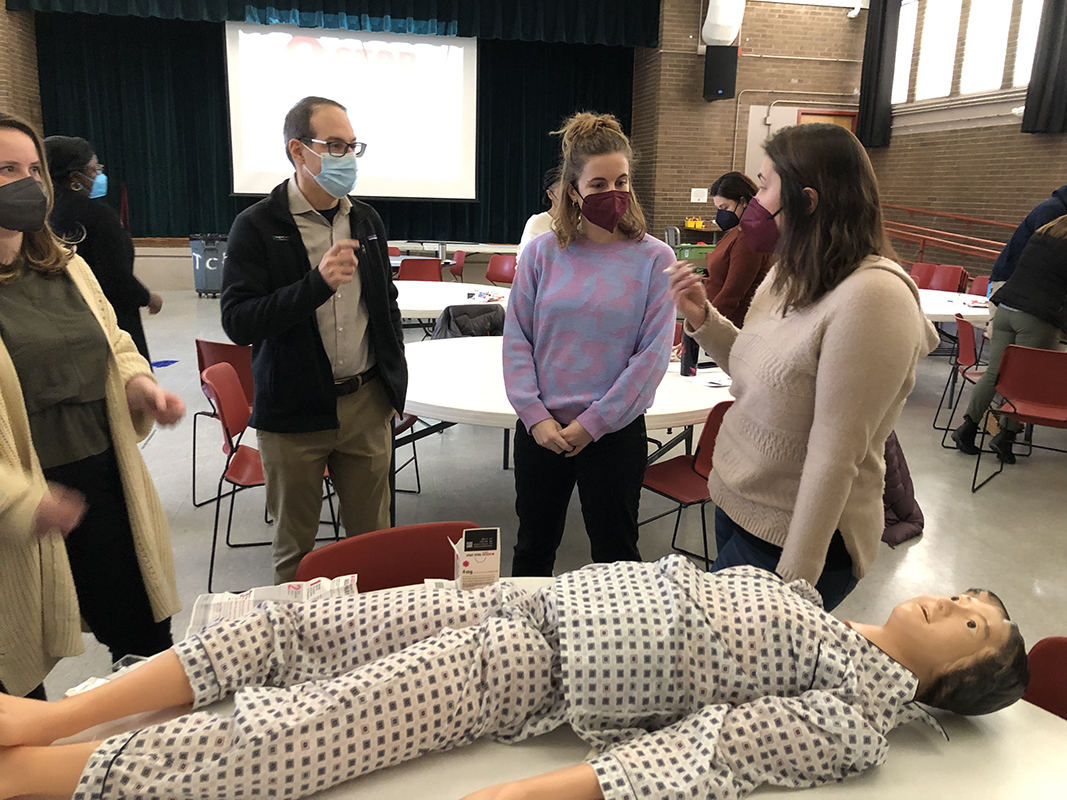
SC: Sure. We talk about the background of opioids in general, the epidemiology, and the statistics. We also focus on the basics of pharmacology–how Narcan works. And then, of course, the practical part is teaching them how to use Narcan. To that end, we have a mannequin, and we show participants how to squirt it in the nose. It’s very simple to do.
But in my mind, the most important thing about the training is acknowledging the stigma associated with opioid use disorder and recognizing just how uncertain people are. Once someone has overdosed on drugs, what do you do, and how do you approach them? This presents an opportunity to talk honestly about harm reduction and make the case that you’re not going to cure someone of their addiction. When they’re ready, we get them to recovery … but you can’t recover if you’re dead. The first step is to save their life.
“The most important thing about the training is acknowledging the stigma associated with opioid use disorder and recognizing just how uncertain people are.”
For the course we just completed, we gave everyone a Narcan kit, which I thought was great. It’s also kind of neat because those have the just-in-time instructions right on the package.
DW: We talk about STOP THE BLEED®–the other element in the layperson empowerment training—in another interview [link]. Knowing that STOP THE BLEED has trained more than 1.5 million people worldwide, I wondered if there were any similar large-scale efforts with Narcan training?
SC: STOP THE BLEED has approved tourniquet devices and a course developed by the American College of Surgeons. They even have a “train the trainers” program. But Narcan is a totally different story because it’s a prescription medicine. Who pays for it? And once you have it, what do you do with it?
I remember attending a debate maybe 10 years ago, where people talked about training laypeople to administer Narcan, and there was a lot of controversy. Fortunately, I think that’s gone away and now there is a vast understanding that it’s an evidence-based intervention. We know that the more Narcan is around in the community, the more lives will be saved.
Regarding large-scale efforts, I am plugged in with the American College of Emergency Physicians and they may be interested in taking this to the next level. There’s also the American Society of Addiction Medicine. However, getting Narcan training to be a part of the BLS [basic life support) training—right up there with CPR training and how to use defibrillators through the American Heart Association or the American Red Cross–would probably be the biggest win.
DW: Do pharmacies offer over-the-counter Narcan?
SC: The FDA has been encouraging over-the-counter Narcan for a long time. Do you know why that isn’t available yet?
DW: I don’t.
SC: It’s the pharmaceutical companies. An over-the-counter price point would probably be about $15 or $20 dollars. But they can charge $100 and get it reimbursed with insurance. And so, even though the FDA has been pushing for over the counter, no company will step up to make it. Still, most states, including Massachusetts, have a “standing order” in which anyone can ask the pharmacist for a kit and can get it without a prescription, and most insurances cover it. Also, there are some new generic versions recently on the market which are helping to drive prices down.
DW: How has the COVID pandemic impacted Narcan access?
SC: Of course, our training programs have been delayed by COVID. But in the last months, we saw the most significant number of overdose deaths in the country that we’ve ever seen. It’s more than 100,000 lives lost. So this is very acute, and it will last far beyond the COVID pandemic.
DW: Dr. Weiner, thank you so much for taking the time to talk with me. Any last thoughts?
SC: Just this: Narcan is expensive. It costs $50 – $70 per kit to get it in the hands of our community partners, which translates to $500 – $700 for each community training. The Stepping Strong Center has generously provided enough funding for four training sessions. We are now seeking additional funds to continue this critical program and are always grateful for additional support.
Scott G. Weiner, MD, MPH, FACEP, FAAEM is an associate professor of Emergency Medicine at Harvard Medical School and the chief of the Division of Health Policy and Public Health in the Department of Emergency Medicine at Brigham and Women’s Hospital in Boston. He is board-certified in emergency medicine and addiction medicine. He is the director of B-CORE: The Brigham Comprehensive Opioid Response and Education Program, a hospital-wide, multi-disciplinary quality assurance program with the goal of reducing opioid-related morbidity and mortality.
