A Conversation with Stepping Strong Research Scholar Dennis Orgill
It’s easy to overlook how much skin works to keep us alive. Experiencing a traumatic wound changes that perspective completely, according to Stepping Strong Research Scholar Dennis Orgill, MD, PhD, plastic surgeon and medical director at the BWH Wound Care Center. Read on to learn how the Stepping Strong Research Scholar team is exploring the next promising advances in wound care to benefit trauma patients.
Q: What is your team working on now to improve wound healing?
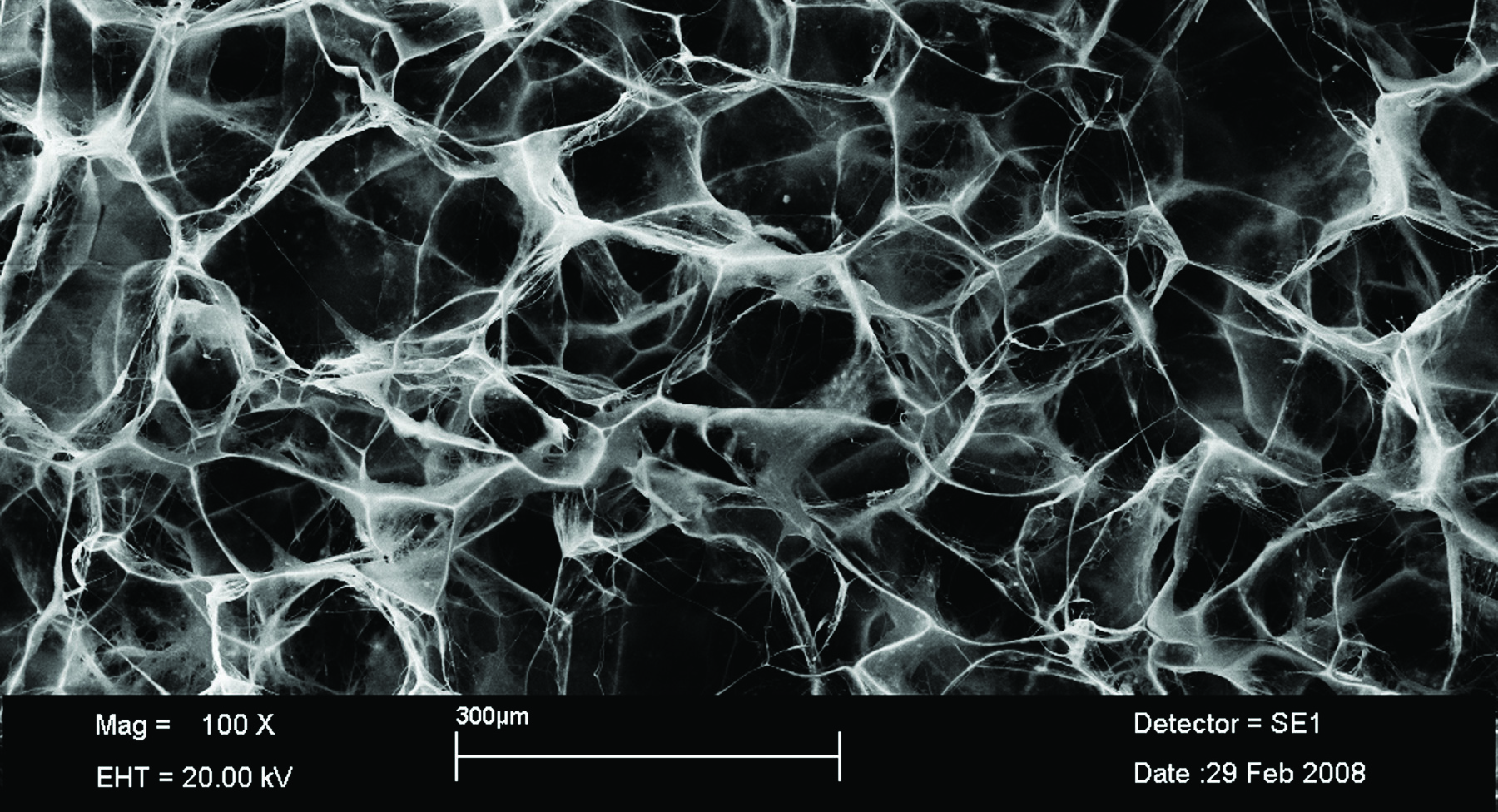
A: The complications from wounds can be devastating—many amputation cases actually start from a wound that doesn’t heal correctly. Our work focuses on a combination of advanced stem cell technologies and dermal scaffolding—a protective template that degrades as tissue regenerates, also called dermal regeneration templates—which we believe is the key to developing better methods for regenerating skin and healing wounds for all types of traumatic injuries. We want to dramatically reduce pain, and significantly reduce the risk of infection.
Q: Are there any challenges to repairing wounds that haven’t yet been solved?
A: We pay a lot of attention to outer recovery of the skin, particularly when donor tissue is involved. But so far no one has achieved restoration of other important aspects that we often take for granted with healthy skin, like hair follicles or sweat glands. This would be a real breakthrough in the field.
Q: In your research, you have found a specific stem cell that shows promise for regenerating tissue. Could you describe how that might be important to the future of trauma care?
A: One of the major research efforts underway at the hospital right now is to see how we can make donor skin tissue immuno-privileged, or engineered to last longer after implantation. We are adding to that volume of work by investigating a stem cell called ABCB5, which is part of the dermis layer and has regenerative and anti-aging properties.
“One of the major research efforts underway is to see how we can make donor skin tissue engineered to last longer after implantation. We are adding to this volume of work by investigating a stem cell called ABCB5, which has regenerative and anti-aging properties.”
Q: Do you have patients who have already benefitted from these innovations?
A: We have treated many patients at the Brigham with dermal regeneration templates, which have been effective in burns, cancer treatments, and chronic wounds.
Q: The team approach is instilled in the culture here at BWH. How important is collaboration to your work?
A: We are at the center of a very robust research community here, and in the Wound Center in particular we have access to thought leaders in vascular surgery, orthopedics, infectious disease, pain management—enough specialties that we can attack wound research from every perspective. Take the example of ABCB5—this research wouldn’t be possible without close collaboration between my group and other experts across the Brigham, especially Dr. Markus Frank in the Division of Renal Medicine, Dr. Natasha Frank in the Division of Genetics, and Dr. George Murphy, who is the director of dermatopathology.
Q: Why is philanthropy so important to your progress?
A: Grants do not always make provisions for this kind of work, even though it has so much potential to change wound care. Having the support of the Stepping Strong Fund means we can pursue this line of research and put our discoveries on a fast-track to clinical practice.
